The Inflammation in the Body
 Get ready for the health buzzword of the decade: inflammation. A key biochemical process inside every one of us, inflammation is the cornerstone of health and healing — and yet — unless you learn the secrets to managing it — it will also probably eventually kill you.
Get ready for the health buzzword of the decade: inflammation. A key biochemical process inside every one of us, inflammation is the cornerstone of health and healing — and yet — unless you learn the secrets to managing it — it will also probably eventually kill you.
The good news: As scientists slowly but surely uncover how the inflammatory response works, they’re learning how we can influence it to our benefit.
Here are five surprising — and life-changing — facts.
Inflammation surprise #1: Inflammation is both your body’s best friend — and its worst enemy.
Inflammation is what happens when a bee stings, a paper cut slices your skin, or pollen or a virus land up your nose. Your body reacts. More specifically, your white blood cells issue a short-term response to defend your body against the assault and help it heal. So far, so good.
Unfortunately, sometimes this process goes haywire. In a classic “too much of a good thing,” certain triggers create chronic inflammation — the body’s defense team doesn’t quit. Immune cells never wind down, causing damage to various body systems and, ironically, leaving them more vulnerable to attack.
Why it’s important
“Inflammation is the basic mechanism that maintains the well-being of our cells,” says Janko Nikolich-Zugich, chair of the department of immunobiology at the University of Arizona College of Medicine and codirector of its Arizona Center on Aging. “But pretty much every disease is also connected to it.”
Luck (good or bad) is a factor; some people are genetically prone to inflammation overload, Nikolich-Zugich says. But within the span of your genes, you have a lot of individual control, he adds. “The key is to have well-controlled inflammation, to keep it regulated so that it switches on when you need it and switches off when you don’t need it anymore.”
Action step: Consume healthier fats.
Fats we eat are the building blocks of both proinflammatory hormones (needed to fight the invader) and anti-inflammatory hormones (needed to calm down the healing process after the wound or other threat is gone), says Beth Reardon, director of integrative nutrition at Duke University. We need both kinds.
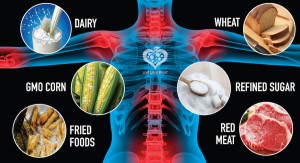
The trouble: We live in such an inflammatory environment (from pollution, germs, diet, and other sources) that it’s tough to keep the inflammation process in balance. The best way to do this is with diet: Decrease the inflammatory fats you eat (called omega 6s, found mostly animal fats from meat and dairy) while increasing anti-inflammatory fats (called omega 3s, found mostly in cold-water fish such as salmon and herring or in fish-oil supplements).
A tricky point: You need two kinds of omega 3s. There are long-chain omega 3s (from fish) and short-chain omega 3s (from flax, seeds, and fortified products, like omega-3 eggs or juice). The two types work in different ways in the body. “People think if they eat foods fortified with omega 3s, they’re doing enough. But most people don’t get enough long-chain omega 3 fats,” Reardon says. Eating cold-water fish twice a week does the trick.
Beware Inflammatory Foods and Extra Weight
Inflammation Surprise #2: Chronic Inflammation Contributes to Almost Every Major Disease
Most people have heard of so-called autoimmune diseases, when the body turns on itself with a hyperactive defense mechanism. Common examples include hay fever, rheumatoid arthritis, gout, pelvic inflammatory disease, colitis, and bursitis.
You can add to this list cancer, Alzheimer’s disease, type 2 diabetes, hypertension, heart disease, Parkinson’s, osteoporosis, and even depression. Many researchers also now believe that inflammation isn’t just a result of osteoarthritis; it may be a contributing cause. “The one thing that unifies most major diseases is inflammation,” says the Arizona Center on Aging’s Nikolich-Zugich. “Whether inflammation is the root cause or whether these diseases are made worse by the inflammatory process isn’t entirely clear yet — but inflammation is almost always a factor.”
Why it’s important
Scientists believe that the key to extending lifespan and late-life well-being lies in figuring out how to manipulate and cut off chronic inflammation. While all the diseases listed above manifest themselves in the body in very different ways, they seem to share many commonalities down at the cellular level.
Action step: Eat a more anti-inflammatory diet.
Because our bodies are exposed to more damage at the cell level than they can handle — a process called oxidative stress — shoring up defenses is key. And there’s no easier way to do that than by carefully choosing what we eat and drink.
What foods contain the most antioxidants? You needn’t be a chemist. Just think three words: color, taste, aroma. In whole (not processed) foods, these traits signal high-antioxidant chemical content, Duke University’s Beth Reardon says. This means:
- Bright or deep-hued fruits and vegetables (berries, eggplant, purple grapes, sweet potato, dark green leafy veggies)
- Foods with strong flavors (bell pepper, watermelon, tomatoes, cruciferous vegetables)
- Foods with powerful odors (garlic, onion, chives)
Other beneficial foods: the spices turmeric, ginger, cinnamon; curry; tart cherries; green tea; red wine; dark chocolate. These help inhibit the formation of inflammatory prostaglandins and COX inhibitors (the same enzyme-inhibiting substances in medications such as Vioxx or Celebrex).
At the same time, avoid highly processed foods full of sugar and saturated fats. These so-called high-glycemic index foods (chips, cookies, crackers, cakes) pour sugar into the bloodstream, upping inflammation.
Inflammation Surprise #3: It’s Not the Look of Your Body Fat but What’s Inside it That Really Hurts You
Little wonder obesity is linked with so many damaging diseases, from diabetes to Alzheimer’s. In just the past five years or so, researchers have discovered that being overweight is a huge cause of inflammation.
“We tend to think of body fat as an inert, annoying consequence of eating too much and not exercising enough,” Beth Reardon says. “We need to think of it as what it really is: metabolically active tissue that’s actually a source of the compounds that trigger inflammation.”
Why it’s important
Having too many extra fat cells basically amps up the inflammatory process. That’s because fat cells are producers of hormones, such as estrogen and leptin, and other molecules that signal the immune system. Excess fat creates excess inflammation.
Belly fat (accumulated around the abdomen) may be especially dangerous, compared with fat in the hips or rear, because midsection fat tends to produce even more estrogens and inflammatory compounds called cytokines, Reardon says.
There’s a silver lining to perimenopausal weight gain, though, she adds. A stubborn muffin top may be nature’s way of trying to hang onto estrogen when hormone levels shift as the ovaries close up shop, in order to protect heart health and make symptoms like hot flashes less severe. (Postmenopause, though, you still want to maintain a healthy weight.)
Action step: Aim for a healthy weight.
Possibly the single best health move you can make: Keep moving. Why? In addition to burning fat and warding off unhealthy fat cells, vigorous exercise three to four times a week subjects the body to controlled stress. That trains the immune system to deal with high-energy demands followed by lower, maintenance levels of functioning. “This allows inflammation to recalibrate,” says Janko Nikolich-Zugich.
Exercise also produces hormones like endorphins, which make you feel good and therefore encourage you to continue this important, immune-boosting activity.
How Stress and Allergies Affect Inflammation
Inflammation Surprise #4: You Can’t Control Everything That Trips Inflammation — but You Might Want to Conquer That Fear of Public Speaking
Inflammatory agents (things that set off our immune system) are all around us — in the air we breathe, the UV rays we absorb, the cleaning agents we use, the makeup we wear, the candles we light, the germs we encounter.
Another surprising source of chronic inflammation: chronic (long-term) stress. Know how some faces flush and palms sweat before the person gives a speech? That’s an inflammatory response. So is breaking out in hives during an argument, or getting a headache and racing heart when pulling an all-nighter.
Why it’s important
In concentrated doses, emotional stress is no big deal. But when the stress is constant — as when dealing with a ongoing personal crisis — it trips a constant inflammatory response.
You can’t control the fact that your aging skin or gut may be a “leaky barrier,” for example, letting in more invaders that cause the body to mount an inflammatory response, Nikolich-Zugich says. Also, as we age, changes to the immune system itself may make it harder to fight familiar bugs and viruses. But, as with diet and exercise, emotions and stress are areas most people can control. And when it comes to inflammation, the body needs all the help it can get.
Action step: Sweep your life of stressors as much as you can.
In addition to following basic advice about using sun protection, washing your hands, exercising, eating an anti-inflammatory diet, and avoiding known toxins (don’t smoke and don’t live with someone who does!), it pays to curb your emotional stress as much as you can.
Some areas many overlook:
- Don’t scrimp on sleep.
- Get depression symptoms treated; it’s a form of chronic stress on the body.
- Know that short-term anxiety is unavoidable, but seek confidence-building help if you’re constantly in an edgy situation (the frequent flyer who hates to fly, the CEO who’s terrified of public speaking).
Inflammation Surprise #5: Many of Us Have Infections and Allergies we Don’t Know About, Which Send Us Into a State of Constant High Inflammation
Here’s a classic case: Someone has inflammatory bowel disease, migraines or other chronic headaches, chronic fatigue syndrome. The various maladies are treated with medications, but the underlying cause of the problem — an undiagnosed food sensitivity, for example — goes untreated. Get to the root of the problem (the food sensitivity upsetting the balance of bacteria in the gut, say) and you’re closer to a cure.
Our medical system tends to treat specific issues rather than the whole person. “When things go wrong, we take something to fix it, instead of trying to control the underlying cause: inflammation,” integrative nutritionist Beth Reardon says.
Why it’s important:
Up to 40 percent of the population has a gluten sensitivity, Reardon says. That’s different from a full intolerance (celiac disease), but enough to notice brain fog, bloating, gastric distress, or fatigue after eating wheat. Dairy sensitivity (lactose intolerance, which is short of true milk allergy) is similar. Both sensitivities tend to grow more common as people get older.
Human bodies evolved to eat dozens of grains, but modern society focuses on one — wheat — and a high-gluten type at that (all the better for fluffy bread and crispy snacks). The problem: Protein in wheat risks irritating the gut (where the immune system mostly begins), causing inflammation. Substances the body believes shouldn’t be there aren’t absorbed well; instead, these undigested proteins work their way into the bloodstream, where the white blood cells react as if they were a virus or any other foreign substance.
Ditto with milk: We evolved to consume fatty breast milk for the first years of life, not to subsist on milk, cheese, and ice cream. Too much of these foods overwhelm a system that’s sensitive to them.
Action step: Pay attention to what your body’s telling you.
You can tell if you have a food sensitivity by how your body reacts. Try eliminating a food type (wheat, dairy, soy, meat) for two weeks. See how you feel. Do symptoms disappear or fade? Now add back the potential allergen and see what happens.
Avoid writing off uncomfortable reactions to fibromyalgia or migraines or some other specific disorder until you’ve experimented with the possibility of a more global root cause. Even if you don’t have a food allergy, replacing problematic foods with the healthier options within a low-fat, plant-based, Mediterranean-style diet will be a win-win for your body.